In any exam, some questions can make you think a bit more deeply. It extends beyond the literal requirements of the exam syllabus. In this series, I write articles exploring topics touched on by such exam questions. I teach in the English-speaking Caribbean, so the syllabi that I teach to were developed by the Caribbean Examinations Council (CXC). So, of course, the questions come from CXC exams.
This article was prompted by a question in the CSEC1 Biology Paper 02 exam, held in January 2017.
Question3(d)
”Suggest ONE reason why haemophiliacs may be more susceptible to infectious disease.”
Before we directly answer this question, let’s dig into haemophilia itself.
What is Haemophilia?
This is a disorder that results in the patient having a reduced ability to make blood clots. It is due to the lack of a particular clotting factor.
A (Mostly) Genetic Disorder
The missing clotting factor is a protein, and thus there is a gene for it. The disorder develops when a mutated form of the gene is present. This mutant gene provides instructions for the synthesis of a defective form of the clotting factor. The defective form does not work properly, and the development of blood clots becomes difficult.
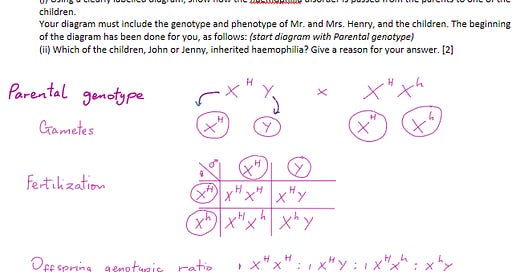
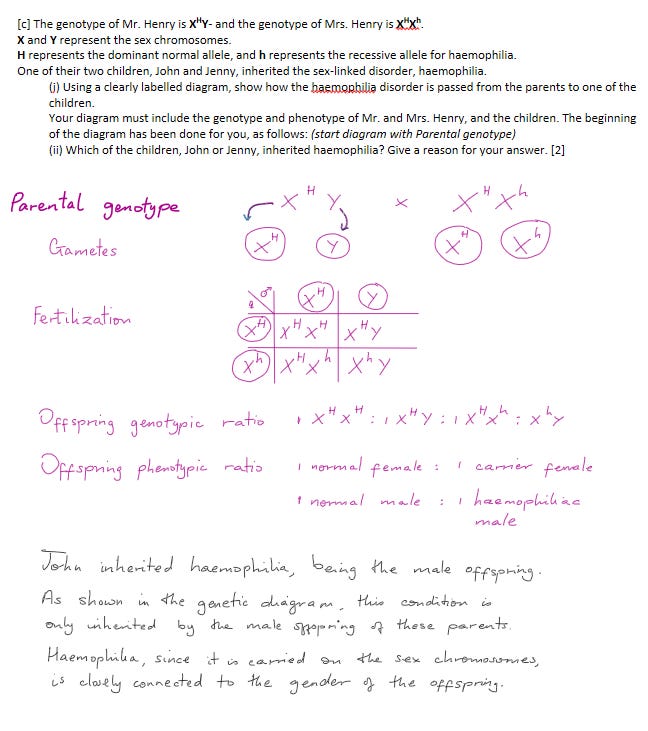
Sex (Gender)-linked
The good news is that the mutant form of the clotting factor gene is recessive.
Why is This Good News?
Every individual carries two copies of most genes. Those two copies don’t have to be identical. Let’s say the pair of genes includes the mutant version and the normal version. Since the mutant gene is recessive, the cell’s protein-making machinery will prefer the normal version, and use it to guide the synthesis of the functional clotting factor. This means that having the mutant gene does not guarantee one will have the disease.
The bad news is that the gene for the clotting factor is on the X chromosome only. It is missing on the Y chromosome.
Why is This Bad News?
Genes are packaged into pairs of chromosomes. Each pair of chromosomes will carry a particular set of genes. The chromosomes that help to determine gender are called X and Y. In females, the pair is XX. In males, the pair is XY.
Therefore, males only have one copy of the gene for the clotting factor. Therefore, if that gene happens to be the mutant version, there is no other gene present to be used instead. So, in males, having the mutant gene guarantees that they will develop the disease of haemophilia.
As a result, the majority of haemophiliacs are males. Females can inherit the disease, but only if both genes are the mutant form, being carried on both X chromosomes.
Advantages of Screening for This Genetic Condition
There are mild forms of this disease. In such cases, patients only discover they are haemophiliac after an accident or during surgery. This kind of sudden revelation can lead to death.
Also, it is important to know one’s condition before having children. A woman can be a carrier for the gene and show little to no symptoms. However, if she has a son, there is a 50% chance of him being haemophiliac, after inheriting the X chromosome with the mutant gene.
Complications
These are the most common complications experienced by persons with haemophilia.
Internal Bleeding
This kind of bleeding occurs deep inside the body - in muscles, joints, or organs. This can cause swelling, pain, numbness, or damage to the affected area.
If this bleeding occurs in the brain or throat, this can be life-threatening.
Joint Disease, aka Arthropathy
This results from repeated bleeding into the joints. In the short term, it produces chronic pain, stiffness, inflammation, and reduced mobility.
In the long term, the joint cartilage and bone wear away, leading to deformity or disability.
Production of Inhibitors
These are antibodies against the clotting factor medicine. They reduce the medicine’s effectiveness or make it completely ineffective. This, in turn, increases the risk of bleeding episodes.
This kind of complication is more common in patients with severe haemophilia.
Infections
Occurs with exposure to blood-borne viruses such as HIV or hepatitis via contaminated blood products or needles. These infections can affect the liver, immune system, and overall health.
Treatment
At-Home Practice
Lifestyle and home remedies essentially focus on avoiding excessive bleeding and protecting the joints. They include the following:
Exercise regularly and maintain a healthy weight. The goal is to strengthen muscles and protect the joints.
Avoid contact sports or activities that can cause injury or trauma. Wear protective gear and clothing when needed.
Avoid certain pain or blood-thinning medications, such as aspirin. These make bleeding worse. Safer alternatives include acetaminophen.
Apply pressure & ice to minor cuts and bruises, to stop bleeding to reduce swelling.
The practice of good dental hygiene. Also regular visits to the dentist, to prevent gum bleeding and tooth decay.
Established Medical Treatments
These are administered within a hospital, usually in a department that focuses on haemophilia and other similar blood disorders.
Regular replacement therapies. These use medicines that are essentially clotting factor supplements. They are used to replace or supplement the clotting factor that is missing or at low concentrations in the patient. These proteins can be extracted from donated blood, or manufactured via recombinant technology.
These medicines can be given to prevent bleeding episodes or to treat them as they occur.
The type and frequency of replacement therapy prescribed for a patient will be determined by:
type and severity of haemophilia
whether inhibitors are present
the patient’s lifestyle and preferences.
Newer and Emerging Treatments
There are newer medications that successfully prevent or stop bleeding without containing clotting factors. Instead, they use strategies such as:
stimulation of the production of native clotting factors. For example, a synthetic hormone called desmopressin. It works by stimulating the production of clotting factor VIII. It is used to treat mild haemophiliacs.
preservation of blood clots once produced. These are called clot-preserving medications or fibrin sealants. These medications tend to be used for minor bleeding, or as part of a larger treatment protocol.
Life Expectancy
This can vary widely, especially across countries. It depends on:
the severity of the condition
the availability and quality of treatment at the location
the presence of other diseases or complications.
Life expectancy has increased by a lot in the last few decades. This is largely thanks to advances in treatment and care. However, on average, life expectancy is still lower than that of the general population. Without treatment, though, patients hardly make it to adulthood.
Note that there was a spike in deaths in the 1980s, due to the HIV and hepatitis infections from contaminated blood products.
In the UK, studies have shown it to be 63 - 75 years.
Studies in the Netherlands gave a median life expectancy of 77 years.
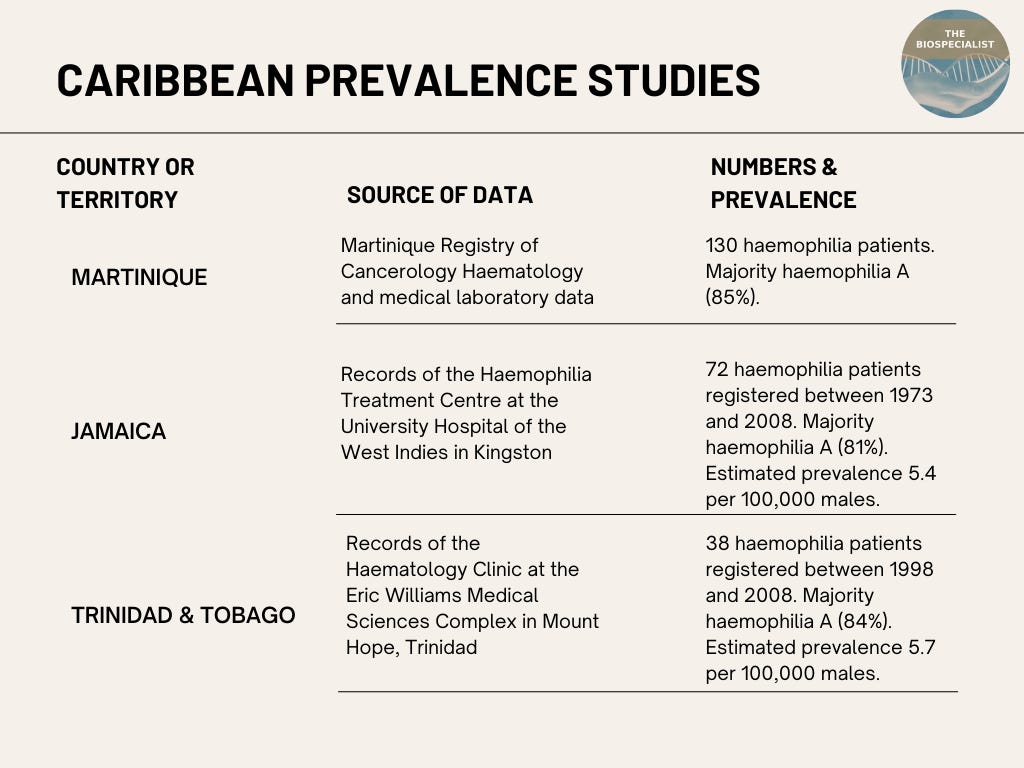
Prevalence
In the Caribbean, the prevalence of this disorder is not well documented. There are limited data sources and registries for the region.
However, studies from specific Caribbean countries and territories suggest that its prevalence is similar to or lower than the global average. However, more comprehensive and updated data is needed.
And Now… We Tackle the Grand Question
Why are Haemophiliacs More Vulnerable to Infectious Diseases?
There are several reasons:
The low level of clotting factors impairs the ability to form clots and to stop bleeding. This leaves wounds open, providing entry points for bacteria to invade tissues and cause infections.
High risk of exposure to blood-borne viruses such as HIV or hepatitis via contaminated blood products or needles. The risk has been greatly reduced in recent times, due to improved screening for blood products and safety measures for injection practices.
Weakened immune systems due to other conditions or treatments that affect their antibody production or complement system. Resources of the immune system may be diverted towards the production of antibodies against the clotting factor medicine. This makes the treatment less effective and thus leads to more bleeding episodes, and increased risk of infections.
They may be exposed to Haemophilus influenzae bacteria through respiratory droplets from infected persons or carriers. This bacteria can cause various infections, such as pneumonia, meningitis, sinusitis, otitis media, and septic arthritis.
REFERENCES
Abacan, D.B. (Nov 17th, 2022). Hemophilia Life Expectancy. AmeriPharma Specialty Care [Blog]. Retrieved 13th June 2023.
Bing AI Chat. (June 9th, 2023). PDF Copy.
Hassan, S. et al. (2021). Mortality, life expectancy, and causes of death of persons with hemophilia in the Netherlands 2001-2018. Journal of thrombosis and haemostasis : JTH, 19(3), 645–653. https://doi.org/10.1111/jth.15182
Mayo Clinic Staff (1). Hemophilia - Diagnosis & Treatment. Mayo Clinic [Blog]. Retrieved 13th June 2023.
Mayo Clinic Staff (2). Hemophilia - Symptoms & Causes. Mayo Clinic [Blog]. Retrieved 13th June 2023.
Pierre-Louis, O.N. et al. (August 2018). Descriptive Epidemiology of Haemophilia in Martinique. WIMJ Open 2018; (2): 47. doi: 10.7727/wimjopen.2017.184. Retrieved 13th June 2023.
CSEC - Caribbean Secondary Education Certificate. Written preferably by students that complete Form 5 in secondary school, which is equivalent to Grade 10 in high school.